Vascular Access for Hemodialysis
Hemodialysis (HD) takes some wastes and water out of your blood. Your lifeline on HD is a vascular access. An access is a way to reach your blood to clean it.

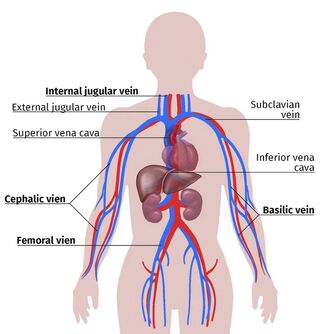
There are three types of vascular access for HD:
-
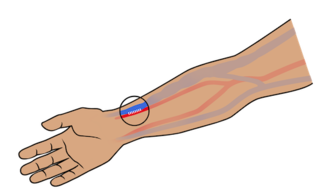
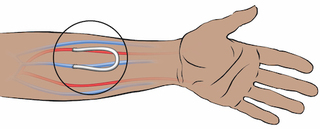
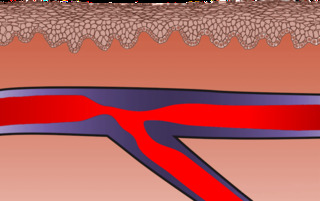
An arteriovenous (AV) fistula. A surgeon links an artery to a vein under the skin of your arm. A fistula is the “gold standard,” becauseit is made only of your own blood vessels. An AV fistula can last for years—even decades. Fistulas are the access least prone to infections and blood clots. Most people can have an AV fistula. If you have a blood vessel disease, a pacemaker, or other health problems, a fistula may not work for you.
-
An AV graft. A surgeon links an artery to a vein under the skin of your arm with a piece of synthetic or bovine (from a cow) vein. A graft is the second best choice. Since it uses tissue that is not your own, a graft is more prone to infection and blood clots than a fistula. Grafts tend to need declotting procedures and a new one must be placed every few years.
-
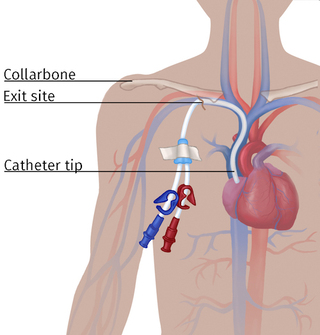
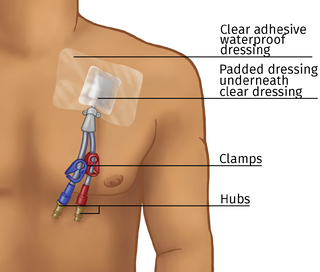
An HD catheter. A catheter is a Y-shaped plastic tube. One end goes in a central vein in your chest and ends in your heart. The other two ends come out through the skin of your chest. Or, an HD catheter can be placed in a large vein in the groin. The biggest plus of an HD catheter is that it can be put in and used the same day. But, since catheters are a doorway into your body, the risk of infection—and death—is far higher. And, HD catheters can wear away your vein or cause narrow spots so you can’t have any other access on the same side. Catheters are best used for only a short time when possible.
There are only about ten sites on the body where an AV fistula or graft can be made:
- The lower arm (most common)
- The upper arm
- The leg.
Fistula or Graft Surgery
You will visit the surgeon to plan for your access first. Bring someone with you if you can, as a second pair of ears. The surgeon should do a painless ultrasound test to “map” your blood vessels. Medicare pays for this, and other health plans may, too.
Ask questions! You may have questions like these:
-
How many dialysis accesses did you do in training? (Studies show that surgeons who did at least 25 do a much better job than those who did fewer.)
-
May I have care tips in writing to take home after the surgery?
-
What should I do—or not do—to help heal?
-
What should I watch out for that could mean there is a problem?
-
What kind of pain medicine will you prescribe for me, and how should I take it?
-
When will I be able to drive?
-
How much weight can I lift? When will that limit change?
-
Will I still be able to play a musical instrument?
-
Can you draw me a picture of what you are planning to do?
You may get your access as an outpatient and go home the same day. The surgery tends to take an hour or so. You may have general anesthesia, and be asleep. Or, you may have just a “local” to numb the site. Some fistulas or grafts need just a small incision (cut) or two. Others have much longer incisions. You may have stitches—or staples—to close your skin back up.
At home, your arm will be swollen, and you will need pain pills for a few days. Keep your arm higher than your heart as much of the day as you can, to help the swelling go down. Resting your arm on a pillow or the back of a couch can help.
To care for a new fistula or graft, do these things each day:

-
Look for redness, swelling, or pus that could mean an infection.
-
Listen for (use a stethoscope) a “whoosh-whoosh” sound called a bruit (brew-ee).
-
Feel for a “thrill” – a buzzing vibration.
-
Never squeeze an access arm with elastic, a watch, or by carrying something across it.
-
Call your care team right away if there is a change—or you have chills or a fever.
Not all access surgery works on the first try. You may need an ultrasound to find problems. A too narrow vein or poor blood flow can be fixed. Sooner is better than later to save an access.

A fistula must “mature” for 4-6 weeks or more before it can be used for HD. As the vein gets blood from the artery, the vessel walls thicken. Light exercise, like squeezing a rubber ball or a hand grip a few times a day, can help. As a fistula matures, it will vibrate. The buzz you feel (thrill ) is a sign of a healthy access. A fistula with no thrill is in trouble. Call the emergency number you were given if your clinic is closed. Study finds that a new device boosts fistula success!
A graft does not have to mature and can be used as soon as it heals (2-3 weeks).
Steal Syndrome
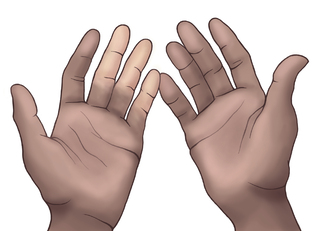
A fistula or graft can “steal” too much blood from the rest of your hand or arm. With “steal syndrome,” your hand might feel cool, turn white or blue, or ache when your access is used. A warm glove can ease a minor ache during HD. If the problem is worse than this, talk to your surgeon. S/he can tie off minor vessels or revise your access. Rarely, people have lost a finger, hand, or arm to an access problem that was not taken care of right away.
Using a Fistula or Graft for HD
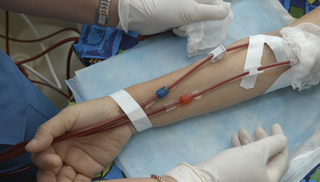
During HD, two large needles are placed in the access. One needle takes blood to the dialyzer (filter). The other needle brings blood back to the body. Since HD is done at least three times a week, how the needles are placed matters! There are three ways to place them—two good, and one bad.
-
It is best to rotate sites for each treatment and move all the way up and down the top and sides of a fistula or graft. At each treatment, needles are placed about ¼ inch away from where they were the time before. This makes a pattern that looks a bit like a rope ladder.
-
The next best way—for fistulas ONLY—is the “Buttonhole Technique.” For 8-10 treatments in a row, sharp needles are placed in the same holes, at the same angle. Tracks form, like pierced earring holes, and guide the needles to the right place. Once the “buttonholes” form, blunt needles can be used. This approach can cause less pain and fewer bumps on a fistula. But, there is a higher risk of blood infection if the scabs from the last treatment are not removed in a sterile way.
-
“Area cannulation” should NEVER BE USED. Placing needles into the same small area over and over will cause weak spots in a fistula or graft. These can bulge out and form large bumps. If the weak spots rupture, death can occur. Know your access and where the needles should go. Learn to put in your own needles to protect your lifeline.
Infiltration
HD needles go through your skin and into the top wall of your access. But, if a needle keeps going through the bottom wall of your access, blood will leak out into your arm. This is an infiltration and it can cause painful bruising that takes days—or weeks—to heal. An infiltration can harm your access.
If this happens, your treatment may stop. A nurse or tech may put pressure on the site and put in a new needle. Use of a cold pack (15 minutes on, 15 minutes off) can help limit the size of the bleed. After 24 hours, a warm pack (15 minutes on and 15 minutes off) can help your body absorb the blood.
You are the only one who can feel both ends of the needle. So, you are the least likely to infiltrate your own needles if you learn how to put them in.
Needle Fear
No one likes needles, but some fear them so much that they avoid health care they need. Or, they are anxious before each HD treatment. Needle fear can make you feel dizzy or faint. Your heart may race. You might even pass out. This is not your fault—and there are ways to help.
Talk with your doctor if you are afraid of needles:
-
Medicare pays for treatment to desensitize you so you are less afraid.
-
Numbing products ease the pain—which can reduce the fear.
-
If you tense and release muscles in your other arm and legs, you may not feel faint.

Or, learn how to put in your own HD needles! (This is self-cannulation.) YOU are the only one who can feel both ends of the needle, so you have the best chance of protecting your lifeline. When you focus on doing it right, it hurts less, too.
Learn more about needle fear and how to cope with it.
Numbing Needles
There are ways to ease needle pain. Your clinic must provide these if you want them:
- Lidocaine creams or gels. These need to soak through the skin, which takes 1-2 hours. Some are prescription and some are over the counter. To use them, wash your access arm with soap and water to remove skin oils. Put on a 1/8” thick layer the size of a dime to each of the two spots where the needles will go. Cover the cream with plastic wrap. Wash the cream off well before treatment.
- Injected lidocaine. A small needle is used to put lidocaine just under the skin. This may burn a bit. Some nurses say that, over time, this product can make the skin over an access tough.
- Ethyl chloride spray. This refrigerant is sprayed onto an access to “freeze” the skin over it.
How a Fistula or Graft Looks and Feels

A fistula or graft can help you live longer on HD. But, if people see it, they may ask you about it. Kidney disease is mostly hidden—people don’t know you have it unless you tell them. But, a fistula or a graft can show, and this is something you will need to get used to.
Besides a scar on your arm, a fistula is a large vein. This is normal and a sign of a good, healthy lifeline. But, people may see it and ask about it. The needle marks can show, too. And, it can take you time to get used to the buzzing of a healthy access. A graft is not as large, but can show as a large line or loop under your skin.

Some people wear long sleeves all year to hide a fistula or graft. Others choose to look at their access as a battle scar of a war they are winning with kidney failure. After all, we all have scars. Some use questions about their access as a chance to teach others. Some make up a silly story (“a shark bit me”) to silence those they don’t want to talk to. If you expect questions and think of answers, it may help you to cope with the change in your body when it occurs.
It is normal to be sad about changes to your body. And, it can help you to talk about your feelings. Your fellow dialysis warriors know what you are going through. Your clinic social worker is a resource, too.
Long-term Fistula or Graft Problems
Some challenges with fistulas and grafts take time to develop. Watch for these:
- Stenosis (a narrow spot). Stenosis will slow or even stop blood flow—which can lead to blood clots.
You may be able to tell if you have stenosis in one of three ways:
-
You may bleed longer after an HD treatment.
-
Your pressure readings during treatment may go up.
-
Your bruit sound may be higher in pitch, like a tea kettle.
Stenosis can often be fixed. A vascular surgeon can open up the access and put in a stent (a sort of splint) to keep it open. Needles cannot be placed into a stent. Too many stents may mean it is time for a new access.
- Blood clots. If you can’t hear a bruit or feel a thrill, your access may have a blood clot. Call your vascular surgeon right away. Often, a clot can be dissolved or pulled out.

- Aneurysm (weak spot that bulges out). Large bumps that you may see on a fistula are often aneurysms. You may not like how these look, and that is a reason to ask them to be fixed. But, these spots also have weak walls—and may be at risk of rupture.
Danger signs that mean a surgeon should fix an aneurysm are:
-
Shiny skin—even on a small aneurysm.
-
Loss of pigment over an aneurysm, if your skin is dark.
-
Scabs at needle sites that are raised up, not flat.
Three Steps to Take if an Access Ruptures
If an access ruptures, a LOT of blood can be lost in just a minute or two. Know what to do!
- Put your finger in the hole to plug it. Towels can cause even more blood loss.
- Raise your arm above your head. (Keep your finger in the hole!) This will slow blood flow.
- Get help. If anyone is with you or nearby, have them call 911. If not, you call—but keep your finger in the hole.
What to Expect When a Catheter is Placed
If you need HD right now, you will need an HD catheter. Or, if you have a fistula or graft that needs repair, you will need one. Anyone on HD may need a catheter at some point.
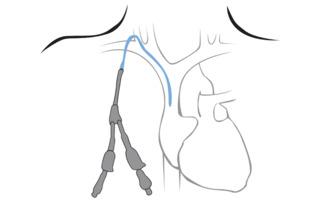
An HD catheter takes 15 to 30 minutes to place. An operating room or a radiology suite may be used. You will be awake, but should get medicine to relax you and ease the pain. A tunnel will be made under your skin by a tool called a trocar. Then, the catheter is inserted over a wire. The wire is pulled out. Then, you will need a chest X-ray to be sure it is in the right spot.
A “temporary” HD catheter will have stitches to hold it in place. These can pull and be uncomfortable. A “Permcath” has plastic cuffs under your skin. Your tissue grows into the cuffs to hold them in place. But, don’t let the name fool you! HD catheters are best used for only a short time, unless you have no other options.
Before you leave, be sure you know:
-
How to change the dressing if it falls off or gets wet. Never use a scissors near an HD catheter.
-
How to clamp the catheter if it starts to bleed.
-
What to do if the catheter falls out or is pulled out by mistake.
To care for a new catheter, do these things each day:

-
Look for redness, swelling, or pus that could mean an infection.
-
Keep your catheter dry. No swimming. No showers unless you use a special cover.
-
Call your care team right away if there is a change—or you have chills or a fever.
HeRO™ Graft
A HeRO™ can be an option for those who can’t have a fistula or graft in an arm or leg. The HeRO uses a piece of graft to link an artery to a vein in the chest. Since it is under the skin, it is safer than an HD catheter.
Using a Catheter for HD
HD catheters do not need needles. For an HD treatment, the dressing is removed. The nurse (or tech in some states) must wear a mask and gloves to take the dressing off. The catheter is looked at to check for signs of infection. The caps are removed and connected to the dialysis tubing.
During HD, a catheter may be “positional.” It may not work as well if you move a certain way. You may need to sit very still during treatment so it keeps working. HD catheter blood flow tends to be less than a fistula or graft. So, an HD treatment may not remove as much wastes and water with a catheter.
How a Catheter Looks and Feels

Having a tube in your chest can be a constant reminder of kidney failure. You can hide an HD catheter under your clothes. It may cause a lump that people may ask about, though. Some people find an HD catheter to be painful, but others do not.
You cannot safely get a catheter wet. This means you may not be able to shower or bathe as often as you might like. There are covers that can help you keep a catheter dry in the shower, but these can be costly.
It is normal to be sad about changes to your body. And, it can help you to talk about your feelings. Your fellow dialysis warriors know what you are going through. Your clinic social worker is a resource, too.
Next Section:
Kidney Transplant
For even more information on Vascular Access
Check out our Kidney School Module on Vascular Acess. Over 24 detailed pages on using your vascular access for dialysis, Needles, how to keep your access clean, and more.
Read our Home Dialysis Central articles
- Hemodialysis Access: Fistula First
- Dialysis Needle Fear - Easing the Sting
- Dialysis Needles, Self-Cannulation and the Buttonhole Technique
- The Art Of Making Your Fistula Or Graft Last
- Blood Pump Speed and Your Dialysis Fistula
- A How-To Manual: The Art of Teaching Buttonhole Self-Cannulation - An article with Video by Stuart Mott, Pioneer in buttonhole cannulation
- How Do You Prevent Indented Buttonhole Sites?

