Options for Dialysis
“When my husband found out he was going on dialysis, I was petrified and he was numb. There are so many unknowns when you start out. All the new terms to learn, diet and fluids, what it will feel like. The only thing that seemed to help us was to start learning—read all the pamphlets from the doctor, ask questions, and hear how others dealt with the disease. It really will be OK. It will be different, but it will be OK.” Juanita L.
“My husband just looks at it like a JOB. This made it so much easier to deal with. Positive thinking helps so much!” Monique S.

The word “dialysis” may sound scary, but it does not mean “die”. Dialysis lets you live. Until the 1960s, if your kidneys failed, you had no options to live. When chronic dialysis started in Seattle, there were too few machines.
“Life and Death Committees” made up of citizens and clergy chose who would get the scarce, costly treatment and who would not. So, you may want to call it Lifealysis, as one young man does. Dialysis can save your life—and change it. Be sure that you can keep doing the things you value most.
 Learn about ALL of the treatments for kidney failure in our 2 minute animated videos.
Learn about ALL of the treatments for kidney failure in our 2 minute animated videos.
How do you choose a treatment when you don’t want any of them? This is what some people with kidney failure ask themselves. We built a tool to make it easier for you -
My Kidney Life Plan
This tool will help you choose the right treatment for you so you can feel your best and live the way you want to. WHAT MATTERS TO YOU?
- Check the values that matter most to you.
- For each value you select, you'll be able to rate how each treatment option fits your life.
- We'll show you a summary when you're done.
Click the image below to help you see how each type of dialysis might affect the things you value most.
How Dialysis Works
To do any kind of dialysis, you need three things:
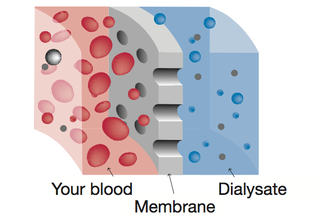
- Access to the Blood. You need a way to reach the blood so it can be cleaned.
- A Semi-Permeable Membrane A membrane is a barrier. In dialysis, it is a thin layer of human or man-made tissue with microscopic pores. The pores let some things pass through the membrane (like water and wastes), but hold others back (like blood cells and protein).
- Dialysate. A mix of purified water and minerals helps to pull wastes and water out of the blood. Dialysate may have some glucose (sugar) in it, too.
During a treatment, blood is on one side of the membrane—with water and wastes in it. Dialysate is on the other side of the membrane. Dialysis works by using chemical principles found in all of nature:
- Diffusion. Wastes will diffuse (pass through) pores in the membrane, because the level of wastes in the dialysate is less than the level in the blood. Diffusion will go on until the waste levels are the same on both sides.
- Osmosis. Water will pass through pores in the membrane, too. This will go on until the level of wastes is the same on both sides of the membrane.
Water Removal in Hemodialysis
Water in our bodies is in three “spaces”—but, dialysis can reach just one of them. Watch this video to see why gentle treatments are best.
There are three “spaces” in your body where water and wastes are found:
Inside Your Cells Each cell is its own bubble, surrounded by a cell membrane. Water and wastes pass in and out through the membranes, which takes time.
Between Your Cells All of your cells float in a sort of “soup” made up of water, salts, and nutrients. Water and wastes pass slowly out of the cells and into this “soup.”
In Your Bloodstream Only about 10% of the water and wastes in your body are in your bloodstream at any given moment.
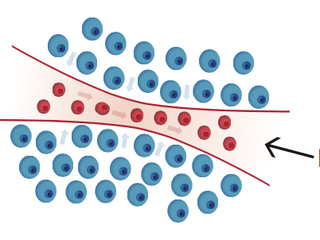
Dialysis can only directly clean your blood. This is a key point—because so little of the excess water and wastes in your body are in your blood. During a treatment, first your blood starts to get cleaner. Then, water and wastes start to move from between your cells into your blood. Last of all, water and wastes slowly shift out of your cells and into the spaces between them. Each of these steps takes time.
Wastes that stay in your body can cause long-term harm to your nerves, bones and joints, and tissues. So, plan to get as much treatment as you can to feel more like you have healthy kidneys. More is better. It’s that simple.
Today, most U.S. citizens can get dialysis. And, most even get help from Medicare to pay for it. Use our calculator to see which treatment will get Medicare to start soonest.
All dialysis is done with the help of a clinic, even if you learn how to do your treatments at home. There are two main types of dialysis: Peritoneal (PD) and Hemodialysis (HD)
Peritoneal Dialysis (PD)
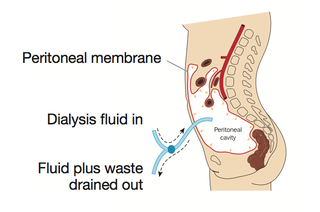
In PD, you use the inner lining of your belly to clean your blood. You fill your belly with sterile fluid through a tube (catheter) placed by a surgeon. During a “dwell” (wait) time, wastes and water in your blood flow into the fluid, which you then drain out. This is called an exchange, and it takes 20 minutes or so.
- Automated PD (APD) uses a cycler machine to do exchanges at night while you sleep. You may also need to do one exchange during the day, by hand.
- Continuous ambulatory (walking around) PD (CAPD) means you do your exchanges by hand. Most people do one around breakfast, lunch, dinner, and bedtime.
 Watch our 2 minute video on Peritoneal Dialysis.
Watch our 2 minute video on Peritoneal Dialysis.


PD and Your Lifestyle

- Most people who do PD use a cycler at night—so their days are free. Some people need a daytime exchange after a while when they have less kidney function left.
- There are no needles with PD, and the exchanges should not hurt. Some people have “drain pain” when they first start to use a cycler. In most cases, this will go away. Some people prefer CAPD.
- If you need to get up during the night, you may be able to get a long drain tube that will let you reach the bathroom or a loved one’s room.
- PD is work-friendly. Your energy level may be constant all day, which can help you keep a job. A manual mid-day PD exchange can be done in a clean room at work.
- You only need to go to the clinic about once a month for blood tests and to meet with your care team.
- Your diet for PD has fewer limits than the diet for standard HD. But, the PD fluid has sugar in it, and you can gain weight if you don’t limit other carbs.
- You can have pets—but they need to stay out of the “clean” room you connect the PD tubing in. It may be best if pets don’t sleep with you at night if you use a cycler.
- Most clinics will not want you to take tub baths or use hot tubs They also will not want you to swim in ponds, lakes, or public pools, due to the risk of infection With a special bandage, you may be able to swim in a private pool With a chest (presternal) PD catheter, you can take tub baths, but many doctors don’t use these.
- Having a PD catheter in your belly (or chest) can change how you feel about your body. Some people have a hard time getting used to this, and it can affect their sex lives.
- PD is travel friendly. You can take a cycler with you for free on an airplane, or put it in the trunk of a car or in an RV. The company that makes the PD fluid will ship it to you for free in most of the U.S.
- If you want to travel to Alaska, Hawaii, or out of the U.S., you may have to pay to ship the PD fluid.
PD Training
Training to learn PD may take a week or so. A nurse will teach you how to safely do an exchange, run a cycler, and order supplies. S/he will come to your house and help you get a room set up for treatment. And, you can call your nurse 24/7 if you have questions.
To learn more about PD:
- Visit Home Dialysis Central
- Watch How to Have a Good Future with Kidney Disease: Dialysis and Your Lifestyle
- Visit Kidney School module 2 - Treatment Options for Kidney Failure
- Buy our Help, I Need Dialysis! book
- Watch our 2 minute video on Peritoneal Dialysis.
Hemodialysis (HD)

For HD, your blood goes out of your body from an “access” and through a filter (dialyzer). Then, your blood comes back to you. This goes on many times over a few hours, and your blood gets a bit cleaner with each pass. A machine controls flow rates and temperature, and has alarms to keep you safe. You can learn to do HD at home. Or, you can go to a clinic three times a week.
There are three schedules for HD:
| Schedule | Treatments Per Week | Hours Per Treatment | Total Hours | Home? | Clinic? |
|---|---|---|---|---|---|
| Standard |
3
Mon. Weds. Fri. or Tue. Thu. Sat. |
4 (More is better) | 12 | ||
|
Short Daily
(do treatments any time of day) |
5-6 |
2.5-4
(More is better) |
12.5-24 | A few clinics offer this | |
|
Nocturnal
(do treatments while you sleep at night) |
3 in a clinic
or 4-6 at home |
8 | 24-48 |
Home Hemodialysis (HHD)

HD can be done in the comfort and privacy of your own home. A nurse will teach you how. You won’t go home until you are confident that you can succeed. And, you will have 24-hour nurse backup by phone. For home HD, you may need a partner. Medicare will not pay for one; most HD partners are family members or friends. Even if you need a partner, it is best for you both if you do as much of your own care as you can.
 Watch our 2 minute video on Home Hemodialysis.
Watch our 2 minute video on Home Hemodialysis.
More Frequent HHD and Your Lifestyle
Home HD can help you feel in more control and give you a more normal life:
- You may feel well enough and have enough energy to work.
- You may be able to take your machine with you for travel, rather than go to a clinic.
- You can do treatments on your schedule, and go to the clinic just once a month.
- You can eat and drink with fewer limits— or may have no limits with nocturnal HD.
- Any type of home HD can help you sleep better at night than the other options.
- Home or nocturnal HD may allow for a more normal sex life.
- Nocturnal HD may make it possible to have a healthy baby.
- Short daily HD or nocturnal HD helps people live longer (about as long as with a transplant from a deceased donor. This is about three times longer than with standard in-center HD or PD).
- You can do treatments on your schedule.
- Less stress on your heart.
- You may reduce your posts dialysis recovery time.
- You may increase your chance of receiving a transplant.
Home HD Training

Home HD training may take 3 to 6 weeks, depending on which machine is used. A nurse will teach you to safely do the treatments, run the machine, and order supplies. S/he will come to your house and help you get a room set up, and will be there for the first home treatment.
To learn more about home HD:
- Visit Home Dialysis Central
- Watch How to Have a Good Future with Kidney Disease: Dialysis and Your Lifestyle
- Visit Kidney School module 2 - Treatment Options for Kidney Failure
- Buy our Help, I Need Dialysis! book
- Watch our 2 minute video on Home Hemodialysis.
In-center HD
You can also do your treatments in a clinic, where you would spend dialysis time with others whose kidneys have failed. Depending on where you live, you may have one or more choices of clinics to work with. If so, you can look up each clinic online to see how well it is doing at projects.propublica.org/dialysis/. Call and set up a tour of the best clinics to see what you think. Look for a clean, friendly place where people get along well with each other. Bring questions with you. See how they treat you when you visit.
 Watch our 2 minute video on In-Center Hemodialysis.
Watch our 2 minute video on In-Center Hemodialysis.
In-Center HD and Your Lifestyle

- If you choose in-center treatments, you must make the biggest changes to your lifestyle:
- Treatments may be done during the work day. This can make it hard to work.
- You go to and from the clinic three times a week (Mon.-Weds.-Fri. or Tues.- Thurs.-Sat.) for treatments.
- You can set up treatments somewhere else when you want to travel. (The social worker can help you reserve a time slot.)
- You will have limits on fluid, phosphorus, sodium, and potassium. And, you may have other diet limits (i.e., for diabetes or heart disease).
- Most people who use this treatment (74%) find that they don’t sleep well.
- Many people who use this treatment also find that their sex lives are affected.
- Of those ages 20 to 29 years old using this option in the U.S., 56.2% lived for 10 years. By age 60, 8.3% lived that long.
However…
- In-center nocturnal HD gives you twice as much treatment. It is much more gentle.
To learn more about In-center HD:
- Visit Home Dialysis Central
- Watch How to Have a Good Future with Kidney Disease: Dialysis and Your Lifestyle
- Visit Kidney School module 2 - Treatment Options for Kidney Failure
- Buy our Help, I Need Dialysis! book
- Factsheet
- Watch our 2 minute video on In-Center Hemodialysis.



